Symptoms and Causes of Ankle Bursitis

Ankle bursitis occurs when the bursae sacs in the ankle become inflamed, causing significant discomfort and mobility issues. Bursae are small, fluid-filled sacs that act as cushions between bones, tendons, and muscles, reducing friction and facilitating smooth joint movement. These sacs can become irritated or inflamed, typically due to overuse, trauma, infection, or medical conditions like gout or rheumatoid arthritis. Common symptoms of ankle bursitis include pain and tenderness in the ankle, swelling, stiffness, warmth, or redness around the affected area. Aching or throbbing pain also can occur, especially when pressure is applied. Overuse from activities like running or dancing, trauma from injuries, or wearing poorly fitting shoes are frequent causes. Proper diagnosis may include imaging tests like X-rays or MRIs to rule out other conditions. In some cases, fluid from the bursae might be tested for infections. If you're experiencing symptoms of ankle bursitis, it is suggested that you make an appointment with a podiatrist for a diagnosis and treatment.
Ankle pain can be caused by a number of problems and may be potentially serious. If you have ankle pain, consult with Nrup Tolat, DPM from Atlanta Total Foot & Ankle Care. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Ankle pain is any condition that causes pain in the ankle. Due to the fact that the ankle consists of tendons, muscles, bones, and ligaments, ankle pain can come from a number of different conditions.
Causes
The most common causes of ankle pain include:
- Types of arthritis (rheumatoid, osteoarthritis, and gout)
- Ankle sprains
- Broken ankles
- Achilles tendonitis
- Achilles tendon rupture
- Stress fractures
- Bursitis
- Tarsal tunnel syndrome
- Plantar fasciitis
Symptoms
Symptoms of ankle injury vary based upon the condition. Pain may include general pain and discomfort, swelling, aching, redness, bruising, burning or stabbing sensations, and/or loss of sensation.
Diagnosis
Due to the wide variety of potential causes of ankle pain, podiatrists will utilize a number of different methods to properly diagnose ankle pain. This can include asking for personal and family medical histories and of any recent injuries. Further diagnosis may include sensation tests, a physical examination, and potentially x-rays or other imaging tests.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are rest, ice packs, keeping pressure off the foot, orthotics and braces, medication for inflammation and pain, and surgery.
If you have any questions, please feel free to contact our offices located in Woodstock and Atlanta, GA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Various Causes of Ankle Pain
Ankles are joints that connect bones in the feet with bones in the lower leg. They are comprised of bones, ligaments, muscles, tendons, blood vessels, and nerves. The ankle joint allows the foot to move side-to-side, as well as up-and-down.
Ankle pain can be caused by a variety of conditions, but is most commonly due to soft tissue injuries such as ankle sprains and strains.
An ankle sprain occurs when one or more of the strong ligaments that support and stabilize the ankle become overly stretched or even torn if the ankle rolls, turns, or twists awkwardly. Depending on the grade of sprain (mild-moderate-severe), there will be varying degrees of pain, swelling, and restricted range of motion, along with tenderness, bruising, and ankle instability. There may even be an audible popping noise at the moment of injury.
Ankle strains can sometimes produce similar symptoms of pain, swelling, and loss of motion, however, they are due to overly stretched muscles and tendons—not ligaments. Ankle strains may also cause muscle cramps in the feet, calves and shins.
Ankle fractures are another common source of ankle pain and occur one or more of the three bones in the ankle become fractured (broken). These breaks can be stress fractures (due to repetitive stress) or traumatic fractures (due to an acute injury). Depending on where and how severe the fracture is, symptoms can include pain and swelling that can sometimes spread up to the knee, bruising or discoloration, and an inability to bear weight. A visible deformity or exposed bone may occur in severe fractures.
Various forms of arthritis may also cause ankle pain. Rheumatoid arthritis (RA) causes the immune system to attack healthy joints, like the ankle joint, by mistake, causing stiffness and swelling in both ankles. Osteoarthritis occurs when cartilage covering the ends of bones wears down, causing the bones to rub against each other. This results in pain, stiffness, and reduced range of motion in the ankle. Gout is a form of arthritis where excess amounts of uric acid in the bloodstream crystallize and build up on joints, causing severe pain and swelling. Reactive arthritis causes joint pain and swelling in the ankle in response to an infection in another part of the body.
Other forms of ankle pain include bursitis (an inflammation of a cushioning bursa sac between tendons and bone), scleroderma (a thickening of connective tissues), chronic ankle instability (caused by improperly healed ankle sprains), Achilles tendon injuries, flat feet, or an infection in the ankle.
Foot Blisters on Elderly Feet
 Blistering skin lesions on the feet of the elderly can be a common and concerning issue. These lesions, often filled with fluid, can result from various factors, including friction, pressure, and decreased skin integrity associated with aging. The skin of elderly individuals tends to become thinner, drier, and more fragile over time, making it more susceptible to damage and blister formation. Moreover, age-related conditions such as diabetes and reduced mobility add to the risk of blistering skin lesions. Diabetic neuropathy can lead to decreased sensation in the feet, making it harder for individuals to detect and address issues like friction and pressure points, which can eventually lead to blisters. If left untreated, blistering skin lesions can increase the risk of infection and other complications, particularly in elderly individuals with compromised immune systems. If you are elderly and experiencing such blisters, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and treatment.
Blistering skin lesions on the feet of the elderly can be a common and concerning issue. These lesions, often filled with fluid, can result from various factors, including friction, pressure, and decreased skin integrity associated with aging. The skin of elderly individuals tends to become thinner, drier, and more fragile over time, making it more susceptible to damage and blister formation. Moreover, age-related conditions such as diabetes and reduced mobility add to the risk of blistering skin lesions. Diabetic neuropathy can lead to decreased sensation in the feet, making it harder for individuals to detect and address issues like friction and pressure points, which can eventually lead to blisters. If left untreated, blistering skin lesions can increase the risk of infection and other complications, particularly in elderly individuals with compromised immune systems. If you are elderly and experiencing such blisters, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and treatment.
Blisters may appear as a single bubble or in a cluster. They can cause a lot of pain and may be filled with pus, blood, or watery serum. If your feet are hurting, contact Nrup Tolat, DPM of Atlanta Total Foot & Ankle Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters are often the result of friction. This happens due to the constant rubbing from shoes, which can lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
Symptoms
(Blister symptoms may vary depending on what is causing them)
- Bubble of skin filled with fluid
- Redness
- Moderate to severe pain
- Itching
Prevention & Treatment
In order to prevent blisters, you should be sure to wear comfortable shoes with socks that cushion your feet and absorb sweat. Breaking a blister open may increase your chances of developing an infection. However, if your blister breaks, you should wash the area with soap and water immediately and then apply a bandage to the affected area. If your blisters cause severe pain it is important that you call your podiatrist right away.
If you have any questions, please feel free to contact our offices located in Woodstock and Atlanta, GA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blisters
Blisters are small pockets of fluid that occur on the top layers of the skin for several reasons. Friction, burns, and diseases are all known causes of blisters. Smaller blisters are known as vesicles, while larger blisters are referred to as bulla. The fluid inside the bubble can be blood, pus, or serum; which is a clear liquid that protects the skin. In most cases, blisters are not a major health issue, but they can be an indicator of a more serious condition.
Causes of blisters vary. Blisters are commonly caused by wearing poorly fitted shoes that rub against the foot. However, there are many other causes besides from friction; including burns, sunburn, insect bites, frostbite, poison ivy/oak, chemical exposure, impetigo, eczema, viral infections, and more.
Most blisters heal by themselves and do not require immediate medical care. If you have a blister, do not pop it since this may cause infection; it is advised to put a bandage over the blister to protect it. If the blister is large, causes pain, or if you have a fever, it is recommended that you see a doctor who can provide proper care. Blisters are easy to diagnose, and if considered prudent by the doctor, can easily be drained of fluid with a sterile needle as well.
To prevent blisters on the feet, wear shoes that fit properly and don’t cause rubbing. Socks can help prevent friction and it is recommended that you wear them if you are wearing shoes. Hand blisters can be avoided by wearing gloves during activities that cause friction against the hand. If you have a blister that pops, do not remove the dead skin, wash the area, apply antibiotic ointment, and cover with a bandage. It is okay in most cases to not seek immediate medical care for a blister if it was just caused by friction. However, if the blister causes pain or does not go away, it is suggested that you see a doctor for a diagnosis.
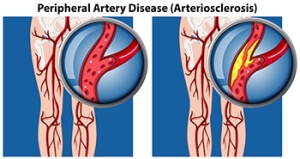
Understanding the Impact of PAD on Foot Health
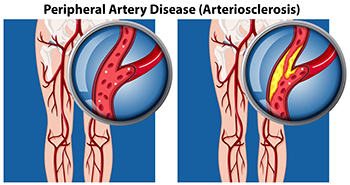
Peripheral artery disease, or PAD, is a prevalent vascular condition characterized by narrowed arteries that limits blood flow to the extremities (including the feet). The restricted blood flow deprives the feet of oxygen and vital nutrients, leading to a range of symptoms. Individuals with PAD may experience intermittent claudication, a condition marked by pain or cramping in the legs or feet during physical activity but subsides with rest. Other symptoms can include numbness, tingling, or weakness in the feet, particularly while at rest or during nighttime. As PAD progresses, individuals may develop non-healing wounds or ulcers on the feet, which pose a risk of infection and tissue damage. Recognizing the symptoms of PAD and seeking timely medical intervention is essential in managing the condition and preserving foot health. Regular exercise, smoking cessation, and medication management are among the strategies employed to lessen PAD's effects and improve overall vascular health. If you have tingling or numbness in your feet, it is suggested that you visit a podiatrist who can diagnose and help you to manage PAD.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Nrup Tolat, DPM from Atlanta Total Foot & Ankle Care. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our offices located in Woodstock and Atlanta, GA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
Differences Between Foot Corns and Calluses

Calluses and corns on the feet are skin conditions that develop as a protective response to prolonged friction and pressure. Although they might appear similar, there are key differences between them. Calluses are broad, evenly thickened areas of skin that typically form on the soles of the feet. They can arise from activities that place repeated stress on this area, such as walking or running in poorly fitting shoes. Calluses have a hard, yellowish appearance and can cause discomfort or pain, making it difficult to walk. In contrast, corns are smaller, more concentrated areas of thickened skin, usually found on the tops and sides of toes. They develop due to the pressure and friction from wearing tight or ill-fitting shoes. Corns feature a dense, central core and can be either hard or soft. Hard corns appear on the bony parts of the toes, while soft corns develop between the toes where moisture keeps them pliable. Both corns and calluses can cause significant pain and discomfort and can lead to infection if not properly managed. Persistent or painful corns and calluses may warrant medical attention. If corns or calluses on your feet are causing you discomfort, it is suggested that you schedule an appointment with a podiatrist for targeted treatment.
Corns can make walking very painful and should be treated immediately. If you have questions regarding your feet and ankles, contact Nrup Tolat, DPM of Atlanta Total Foot & Ankle Care. Our doctor will treat your foot and ankle needs.
Corns: What Are They? And How Do You Get Rid of Them?
Corns are thickened areas on the skin that can become painful. They are caused by excessive pressure and friction on the skin. Corns press into the deeper layers of the skin and are usually round in shape.
Ways to Prevent Corns
There are many ways to get rid of painful corns such as:
- Wearing properly fitting shoes that have been measured by a professional
- Wearing shoes that are not sharply pointed or have high heels
- Wearing only shoes that offer support
Treating Corns
Although most corns slowly disappear when the friction or pressure stops, this isn’t always the case. Consult with your podiatrist to determine the best treatment option for your case of corns.
If you have any questions please feel free to contact our offices located in Woodstock and Atlanta, GA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Corns and Calluses
A corn is a lesion that forms in the skin of the foot, and it is typically circular in shape, small in size, and thick and rough in texture. A corn generally occurs as a result of repeated pressure on the skin; one example of this is the rubbing of a shoe against the skin. Corns differ from calluses in that their central cores are harder in texture.
A corn is a relatively common condition with a wide variety of treatment options. If a corn becomes overly uncomfortable or painful, consult with your podiatrist; he can determine the best method of treatment that is appropriate for you. Corns may return if the underlying cause of its development is not treated or removed. Avoid removing corns at home, as improper removal may cause infection.
A callus, similar to a corn, is an area of skin that has become thickened due to repeated pressure and rubbing. The rubbing causes the skin to create a layer of protective skin, which is the formed callus. Calluses can differ in size between people, and they can also become painful.
Multiple treatments are available for calluses. At-home treatment and removal should be avoided, as this can potentially lead to infection. Your podiatrist can best determine the cause of your calluses and suggest the treatment most appropriate for you.
Causes of Poor Circulation in the Feet
 Poor circulation in the feet and lower legs can be caused by several common health issues that impact blood flow. One of these health issues is peripheral artery disease, or PAD, where arteries narrow due to plaque buildup. This reduces blood supply to the lower limbs and feet. Diabetes can also contribute to circulation problems because changing blood sugar levels damages blood vessels, reducing their ability to transport blood efficiently. Obesity can also contribute by putting strain on the circulatory system, and sedentary lifestyles further hinder blood flow. Smoking is another major risk factor for poor circulation in the feet, as it causes constriction and hardening of the arteries. Symptoms of poor circulation include cold feet, numbness, tingling, swelling, and in severe cases, pain and skin color changes. Regular check-ups with a podiatrist, or foot doctor, can help you manage and mitigate the effects of poor circulation. If you have any symptoms of poor circulation in the feet, it is suggested that you consult with a podiatrist for care.
Poor circulation in the feet and lower legs can be caused by several common health issues that impact blood flow. One of these health issues is peripheral artery disease, or PAD, where arteries narrow due to plaque buildup. This reduces blood supply to the lower limbs and feet. Diabetes can also contribute to circulation problems because changing blood sugar levels damages blood vessels, reducing their ability to transport blood efficiently. Obesity can also contribute by putting strain on the circulatory system, and sedentary lifestyles further hinder blood flow. Smoking is another major risk factor for poor circulation in the feet, as it causes constriction and hardening of the arteries. Symptoms of poor circulation include cold feet, numbness, tingling, swelling, and in severe cases, pain and skin color changes. Regular check-ups with a podiatrist, or foot doctor, can help you manage and mitigate the effects of poor circulation. If you have any symptoms of poor circulation in the feet, it is suggested that you consult with a podiatrist for care.
Poor circulation is a serious condition and needs immediate medical attention. If you have any concerns with poor circulation in your feet contact Nrup Tolat, DPM of Atlanta Total Foot & Ankle Care. Our doctor will treat your foot and ankle needs.
Poor Circulation in the Feet
Poor blood circulation in the feet and legs is can be caused by peripheral artery disease (PAD), which is the result of a buildup of plaque in the arteries.
Plaque buildup or atherosclerosis results from excess calcium and cholesterol in the bloodstream. This can restrict the amount of blood which can flow through the arteries. Poor blood circulation in the feet and legs are sometimes caused by inflammation in the blood vessels, known as vasculitis.
Causes
Lack of oxygen and oxygen from poor blood circulation restricts muscle growth and development. It can also cause:
- Muscle pain, stiffness, or weakness
- Numbness or cramping in the legs
- Skin discoloration
- Slower nail & hair growth
- Erectile dysfunction
Those who have diabetes or smoke are at greatest risk for poor circulation, as are those who are over 50. If you have poor circulation in the feet and legs it may be caused by PAD and is important to make changes to your lifestyle in order to reduce risk of getting a heart attack or stroke. Exercise and maintaining a healthy lifestyle will dramatically improve conditions.
As always, see a podiatrist as he or she will assist in finding a regimen that suits you. A podiatrist can also prescribe you any needed medication.
If you have any questions please feel free to contact our offices located in Woodstock and Atlanta, GA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.